If you have low energy, low sex drive, or mood changes, you might see ads for testosterone therapy and wonder if it could help. Then you see news stories about heart attacks and stroke risk, and maybe an FDA warning, and it suddenly feels scary and confusing.
If you live in Chicago and already see an OB-GYN or primary care doctor on Fullerton or nearby, you might hear different opinions from friends, social media, and even other clinics. Newer large studies, like the TRAVERSE trial, found no increase in major heart events for most men with true low testosterone, but there are still concerns about heart rhythm problems, blood clots, and blood pressure. This guide gives you a simple, balanced overview so you can ask sharper questions at your next visit.
What Testosterone Therapy Is and Who It Is Really For

Testosterone therapy is most often used for men who have both low blood levels of testosterone and clear symptoms, like low sex drive, fatigue, depressed mood, and loss of muscle. The goal is to bring levels back into a healthy range, not to create “super” levels.
You might see this topic on a women’s health site for a few reasons. Your partner could be considering testosterone, you may be in a relationship where hormone changes affect both of you, or you might be a transmasculine patient getting gender-affirming care. Some women are also curious about how testosterone fits into hormone balance in midlife.
At Women’s Health Center of Chicago, most hormone talks focus on estrogen and progesterone for menopause, such as hormone replacement options at WOHCC. Testosterone may still come up in those conversations, so it helps to understand the basics.
How Testosterone Therapy Works in the Body
Testosterone affects energy, muscle mass, sex drive, red blood cell production, and even mood. It also interacts with your blood vessels, blood pressure, and cholesterol patterns. When levels are very low, you can feel like someone “dimmed the lights” on your daily life.
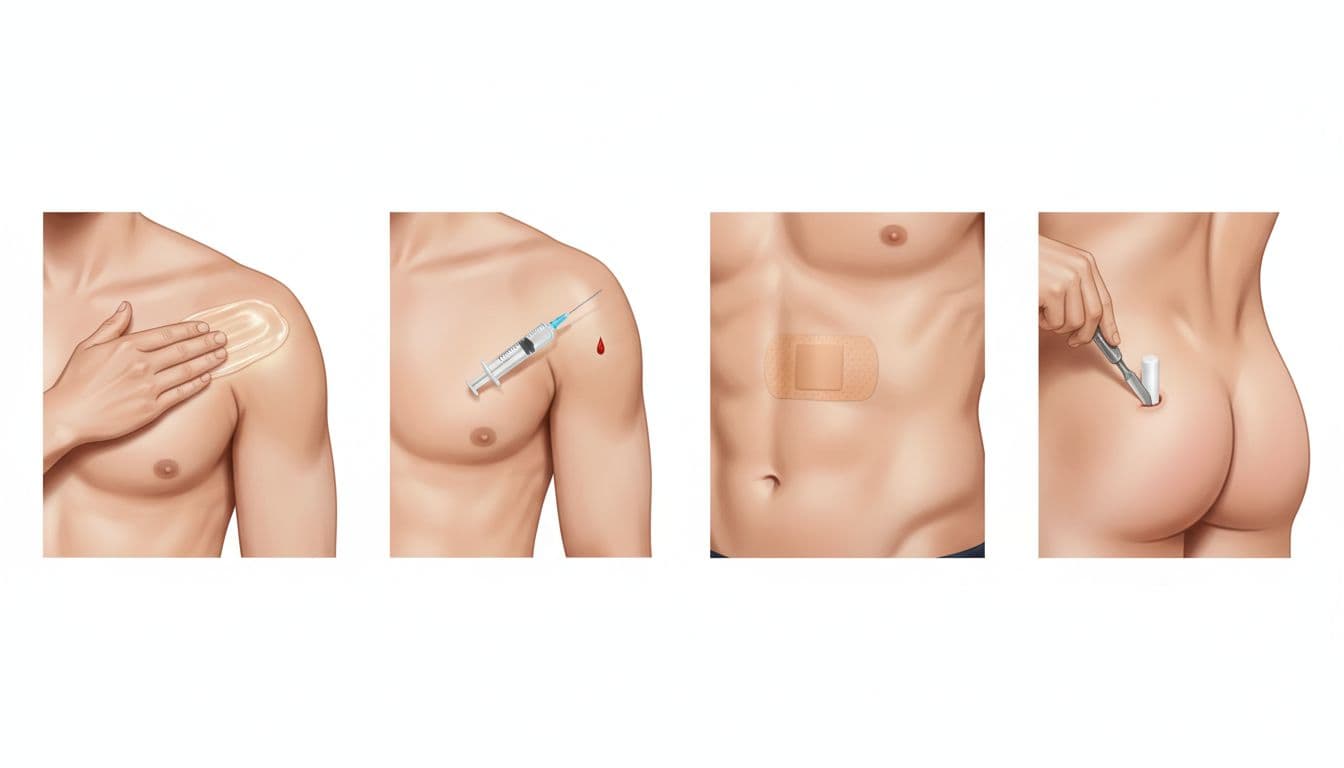
Common treatment forms include gels you rub on the skin, injections, skin patches, and tiny pellets placed under the skin that slowly release hormone.
Who Might Be a Candidate (And Who Is Not)
You are more likely to be a good candidate for testosterone therapy if:
- Your blood tests show clearly low testosterone on at least two morning samples.
- You have symptoms that fit low testosterone, such as low sex drive, fewer spontaneous erections, low energy, or depressed mood.
- Your doctor reviews your medications and health history and does not see a safer explanation or fix.
You are usually not a good candidate if you just want to boost normal aging, build muscle for sports, or increase fertility. Some clinics advertise testosterone as a quick fix for belly fat or low motivation, but real medical use is narrower and more careful.
Some transmasculine patients use testosterone as part of gender-affirming care. For them, heart and clot risks also need close monitoring, often with both an OB-GYN and a primary care doctor involved.
Women sometimes receive very low-dose testosterone for specific problems, such as severe low sex drive after menopause, but that is not routine care. This should only be done by a specialist who understands both hormone and heart risks. If you live in Chicago, your OB-GYN or primary care doctor can help you decide if you need a referral.
How Testosterone Therapy Affects Your Heart and Blood Vessels
This is where the news stories, warnings, and research can feel hard to sort out. Your goal is simple: you want to feel better without taking an unnecessary risk with your heart.
What Recent Research Says About Heart Attack and Stroke Risk
Years ago, some small studies and clinic reports hinted that testosterone might raise the risk of heart attacks and strokes, especially in older men. That led to strong FDA warnings and a lot of fear.
Newer research tells a more detailed story. The large TRAVERSE trial followed more than 5,000 men, many from 45 to 80 years old, who had low testosterone and higher baseline heart risk. Over about 3 years, men who used testosterone did not have a higher rate of major heart events (heart attack, stroke, or cardiovascular death) compared with men on placebo.
One important detail: low testosterone itself is linked with higher heart risk. Men with low levels are more likely to have diabetes, weight gain around the middle, and less physical activity. When testosterone is used correctly, some men feel better, move more, and manage their health more actively. That may help balance out risk in the big picture.
Your Chicago doctor may see testosterone as roughly neutral, or in some cases slightly helpful, for major heart events when it is:
- Used in men with proven low levels.
- Prescribed in standard doses.
- Paired with good follow-up and healthy habits.
Possible Heart Rhythm and Clotting Risks You Should Know About
Even though major heart attack and stroke risk did not increase in big trials, there were other signals you should know about. Some men on testosterone had more atrial fibrillation, which is a fast, irregular heartbeat that can feel like a fluttering or pounding in the chest.
There were also small increases in blood clots in the legs or lungs, and some reports of higher blood pressure. Testosterone can raise red blood cell counts, which can thicken the blood and make clots more likely if levels go too high.
This does not mean you will have these problems, but it explains why screening and follow-up visits matter. Before starting therapy, tell your doctor if you have:
- A history of blood clots, stroke, or transient ischemic attacks.
- Kidney disease or sleep apnea.
- Any heart rhythm issues, even if they were years ago.
FDA Label Changes and What They Mean for You
For a time, testosterone products carried a very strong “boxed” warning about heart risk. After newer trials like TRAVERSE, the FDA removed that box and updated labels.
Labels now focus more on:
- Using testosterone only in men with true low levels, not just aging.
- Explaining that some products can raise blood pressure.
- Advising regular checks of blood counts and heart health.
This update does not mean testosterone is risk free. It means that for the right patient, major heart events do not appear higher over the first few years, as long as you are monitored.
Deciding If Testosterone Therapy Is Safe For Your Heart

You do not have to sort out all this research on your own. A good plan involves your primary care doctor, and in many cases your OB-GYN, especially if you are already working on hormone questions, menopause, or fertility.
If you are in midlife and looking at the full hormone picture, you may also find it helpful to review a broader menopause symptoms and treatment guide so you can see how estrogen, progesterone, and lifestyle tie into long-term heart health.
Questions to Ask Your Doctor About Heart Safety
Bring a short list of questions to your next visit. For example:
- What were my exact testosterone levels, and how low are they compared to normal?
- Do my age, blood pressure, cholesterol, and family history make testosterone higher risk for my heart?
- How will you track my blood pressure, cholesterol, and red blood cell count once I start?
- How often will I need blood tests, and how often should I come in for in-person checkups?
- What symptoms should make me call you right away or go to the ER?
- Are there lifestyle changes or other treatments that might help before or along with testosterone?
Writing these down on your phone or a small card can help you feel more in control during the visit.
Monitoring Your Heart While You Are On Testosterone
If you and your doctor decide to start therapy, you should have a clear monitoring plan. That usually includes:
- Regular blood work to check testosterone level, red blood cell count, and sometimes cholesterol.
- Blood pressure checks in the office and often at home.
- Watching for signs like chest pain, sudden shortness of breath, leg swelling, or a racing, irregular heartbeat.
Call 911 or go to the ER if you have sudden chest pain, trouble breathing, or signs of a blood clot in your leg, such as one calf that is red, swollen, and painful.
If you receive hormone care from an OB-GYN clinic or gender-affirming clinic in Chicago, they may coordinate with your primary care doctor or a cardiologist. Team-based care helps keep your symptoms, hormone levels, and heart health aligned over time.
Conclusion
Testosterone therapy does not appear to raise the risk of major heart attacks or strokes in most men with true low levels, but heart rhythm and clot risks still need careful screening and follow-up. You do not have to sort through mixed headlines by yourself; your doctor can weigh your age, symptoms, labs, and heart history and help you see the real tradeoffs. If you live in Chicago and have questions about hormones, reach out to your local OB-GYN or primary care practice, and remember that daily habits like exercise, not smoking, and a healthy weight still do the most to protect your heart in the long run.



